The Dangers of Benchmarking
Posted on: August 11th, 2009The Dangers of Benchmarking
President, Workforce Prescriptions
Well, it is here . . . ! Healthcare’s pursuit of improved productivity and reduced labor expense has culminated in the inevitable explosion of benchmarking companies ready to identify “over-staffing” and therefore, labor waste. And if your organization needs to rapidly reduce labor expense, this can sure seem like the shortest distance between two points.
Unfortunately, pursuing the recommendations of benchmarking firms can be an extremely dangerous proposition that can leave organizations far worse off than if they had just stayed the course.
To assume that the most effective manner of reducing labor expense is to reduce the availability of labor is to consciously choose to jeopardize:
- employee engagement
- workforce flexibility
- & physician willingness to refer
When you lower employee engagement (and downsizing always does), lower access to labor, reduce workforce flexibility and risk the revenue that physician referrals represent (physicians resent changes in staffing sometimes more than the staff themselves do), you have just created the perfect storm for yourself. Post RIF (reduction in force) audits in healthcare illustrate that any financial benefit derived from a reduction in staff is nearly always lost over the following 30 months. Data further validates that RIF's can foster circumstances where higher paid staff are required to assume the duties of downsized lower paid staff resulting in a raised cost-per-hour of labor within the organization.
Over time, this creates the opposite result of what was intended, and it is not uncommon (post benchmarking visit) to see hospitals paying a $25-40/hr RN to complete the tasks that were previously provided by an $8-12/hr unit secretary. Not only does this take the RN out of direct patient care for a larger amount of time, but it requires that the organization find a way to back-fill the clinical expertise the RN can no longer provide.
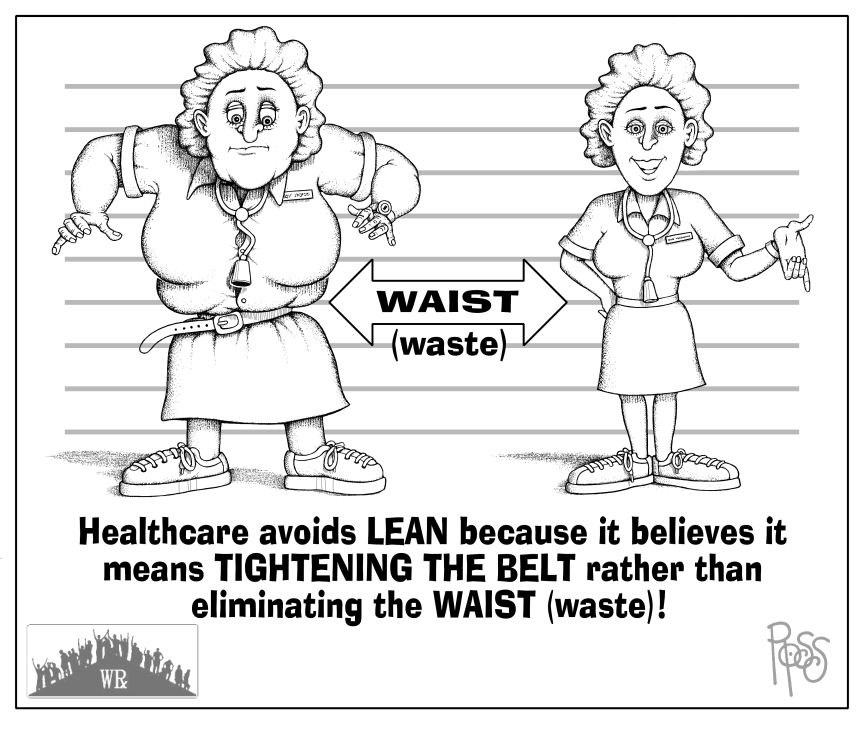
While we have all heard the mantra: No money - no mission, it’s high time for healthcare to begin embracing some of the core productivity, process and business competencies that have become the cornerstone of bottom line performance in other industries. In a market rife with staff shortages, access to labor (having enough of the right kind of staff at the right time) must be preserved.
In the final tally, healthcare isn't like a manufacturing business and patients can't be managed like an assembly line. The only product involved is the productive labor of staff. Staffing benchmarks don't tell that part of the story nor do they describe what outcomes were created by the organization’s whose staffing levels were benchmarked. With 43% of hospitals currently “unprofitable” – what exactly are we comparing ourselves too?
The examples below illustrate these issues clearly.
Example 1: An organization in the Northeast hired a prominent benchmarking company in order to reduce labor expense and improve productivity. The results came back that the organization, in the 16 departments analyzed, could reach the top 25% of the comparison group by:
· reducing staff by over 60 FTE’s,
· reduce overtime by over $600,000
· and reduce Agency/Contract staffing by over $1,500,000
Within these recommendations were specific goals for each department. For the ED as an example, the benchmarking organization has stated that “to be in the 25th %tile”, the ED needed to reduce:
· 7.61 FTE’s and
· over $111,000 in overtime
· over $171,000 in agency
Unfortunately, the analysis provided by the benchmarking provider failed to consider some of the most important operational issues that make up the foundation of how healthcare actually works:
· What % of ED volumes end up admitted in the benchmarked hospitals? (admitted volumes require greater ED time than “treat-and-release volumes”)
· What are the comparable quality measures of the benchmarked hospitals (what clinical outcomes are they producing with these staffing levels)?
· What level of automation do the benchmarked hospitals have? (Let’s face it, highly automated organizations CAN be more efficient)
· Does running this lean ever require any of the benchmarked hospitals to divert? (wouldn’t that be sad – having to divert over staffing choices to meet a benchmark)
· What is the average acuity level of patients in the ED’s of the benchmarked hospitals? What % of the benchmark group's ED volumes are "ambulatory"/"non-emergent" and do they have an onsite ambulatory/fast track option . . . How about a 23 hour observation unit? (what if all their patients are “well”)
· What is the average level of employee engagement of the ED departments that have been benchmarked? (are they burning out/through staff due to an extraordinary work burden/safety issues)
· How long have they sustained the benchmarking performance level . . . Could it have been a fluke? (are you being benchmarked against a “once-in-a-lifetime” event)
· Is the benchmarking compare group data "grossed up" for budgeted and approved (but unfilled) vacancies or is it possible that some/many of the benchmarked hospitals happened to be “lean” due to vacancies they intended to fill? (What if the data isn’t completely valid)
Another Example: An upper Midwest hospital recently hired 3 separate firms to benchmark labor. They were informed by all three firms that they were “over-staffed” in their case/care management team by 15.7 FTE’s.
Some facts:
· The case management department was at the 92nd %tile in staffing (according to the benchmarks) and the organization desired them to be at the 50th %tile.
· They had reduced the organizations LOS from the industry average of 5.2 days to a record setting 3.7 days on very high acuity
· They had done so by optimizing care processes and focusing on truly organizing how care was prioritized and comported. Each patient had case management and social work interaction and discharge & care planning were both being completed at admission.
Unfortunately, what the benchmarking company had failed to do was ASSESS THE RESULTS THE TEAM WAS PRODUCING!
What hadn’t been considered by the benchmarking organization was that the hospital risked becoming average again in results if they pursued average levels of staffing! If this happened, the hospital would add 39,386 uncompensated days per year ($45,311,914 in labor waste).
These are just two of hundreds of examples of the risks that benchmarking represents if not fully understood ahead of time. Below is a simple guide to understanding “why” benchmarking can fail as well as some basic steps to ensure it doesn’t for your organization.
Step 1: Recognize that no two hospitals are alike.
All hospitals have:
- Different physical layouts,
- Different levels of acuity/care,
- Different staffing mixes based upon the unique type of care provided,
- Different vacancy burdens based on local market conditions,
- Different levels of technology,
- Different payor based revenue pressures,
- Different service line structures,
- Different levels of physician employment & alignment,
- Different levels of access to part-time labor,
- Different skill levels of staff . . . and most importantly . . .
Different outcomes generated.
To compare one organization against another based solely on the “number of hours worked per volume” or “cost per hour worked per volume” is equivalent to comparing the speed of an airplane to that of a submarine. They both serve a specific purpose in support of an objective but it is not often the same purpose and not always even the same objective.
Step 2: Recognize that benchmarking works better in some departments
If your organization is considering using benchmarking as a method of identifying labor waste it is extremely important that you approach it on a department-by-department basis and test the broad assumptions the data makes. Departments with higher parallels in volume data (such as those measured by acuity-adjusted-patient-days) who due to industry pressures track similar quality measures (such as: rates of infection, slips & falls, etc . . .) who are sandwiched in the care delivery process (few direct admits or direct discharges) are most likely to benchmark with fewer organizational variances. Conversely, departments on the front or back end of care processes such as ED & obs departments, TCU’s, tend to have the greatest variances. Also to be considered are non-direct patient care areas which may measure different units of work based on organizational variances.
Step 3: Don’t be afraid to ask questions of your data provider in advance
You can avoid much future pain by asking and answering specific questions that highlight the potential differences between your organization and those in the benchmarking pool. If time or political pressure do not allow such detailed introspection (such as was asked of the ED benchmarking conclusions in the example above) then at a minimum, assemble your leadership team and ask the 3 most important questions:
- Is this benchmarking data “actionable” in its current form?
- Does it take into consideration the ways in which we are unique/different from the benchmarked facilities?
- What risks are we taking if we chose to act on this benchmarking data knowing that no quality or results data were included in determining the benchmark?
If you can answer these questions in a satisfactory manner, then you can feel better knowing your benchmarks are not likely to hurt the organization. If, however, you are unable to do so, then take a pause and focus onidentifying the work processes, automation levels or unique operational pressures that drive human behavior and force labor waste in your organization. It is always better to benchmark your current performance against your own best historical performance and address the process challenges that have grown in the meantime than to compare your apple to someone else’s orange!
View All Articles